Precision Medicine Makes it Easy to Get the Right Treatment at the Right Time

When awarding the 2017 Nobel prize for economics to The University of Chicago Professor, Richard Thaler, the committee cited his contributions to the study of human behavior as much as economics. In Thaler's view, changes to people's behavior hinge upon interconnected dynamics of attention and resistance. Or, put another way, small environmental changes can have enormous impacts on the choices we make—and their consequences.
The key mantra from Thaler's groundbreaking book on behavioral economics, "Nudge: Improving Decisions about Health, Wealth, and Happiness" is make it easy. "If you want to get people to eat healthier foods, then put healthier foods in the cafeteria, and make them easier to find, and make them taste better." If you want to get somebody to do something, make it easy!
Precision medicine is a term in healthcare that refers to the tailoring of medical treatment to the individual—in essence, personalizing care based on the precise characteristics of each patient.
These solutions are gaining traction. In a recent Jabil-sponsored survey of more than 200 healthcare decision-makers, three-quarters indicated that their company is either seriously considering options for personalized solutions or are already producing these solutions. Download the full survey.
A view across the healthcare industry through the lens of nudge theory reveals how much of the industry's digital health transformation in recent years has not only been driving more personalization, it is doing so in sync with this orientation toward making things easier: telehealth and remote patient monitoring (RPM); at-home testing; user-friendly health apps; cloud-enabled 24/7 access to medical information; interoperable and connected product ecosystems putting the patient in control.
Let's be clear, the clinical needs of patients are rarely simple or easy. Neither is the responsibility of providers for the consistent delivery of improved medical outcomes. But at a behavioral level, the industry has been increasingly incorporating the voice of the patient, much as other industries have evolved in their pursuit of delighting their customers.
Medical science is complex, intricate and nuanced. But digital health is instrumental in making it easier for healthcare consumers to be healthier and for healthcare providers to deliver better care. With every innovative new connected product, device and platform hitting the market, digital health original equipment manufacturers (OEMs) are heeding the call to make it easy.
Digital Health Fueled by Data
The Healthcare Information and Management Systems Society, Inc. (HIMMS)—an industry advocate and sponsor of the largest health information and technology conference in the world—released a new definition of digital health in March 2020 to serve as a benchmark for the global health community.
Digital health connects and empowers people and populations to manage health and wellness, augmented by accessible and supportive provider teams working within flexible, integrated, interoperable and digitally-enabled care environments that strategically leverage digital tools, technologies and services to transform care delivery.
"Digital health" is essentially a convergence of technologies. Connectedness protocols and processing capabilities provide the means for capturing and communicating ever-expanding digitization of health information. In recent years, personal genomic data has been increasingly added to these files. In parallel, advances in artificial intelligence (AI) and machine learning provide analytic muscle.
The extracted knowledge from within healthcare data is changing the game. If healthcare data is like gold, diagnostics and other information-gathering technologies and devices are the picks, pans and shovels. The payoff is precision medicine, or personalized medicine, as it is sometimes referred to. Driven by the actionable insights unlocked through AI, it's a more predictive and proactive healthcare management strategy for identifying potential health concerns and disease risks early. It's helping physicians and the industry-at-large pivot from simply practicing medicine to practicing health.
What is Precision Medicine?
For each of us, our continued health—as well as our vulnerability to disease and its progression—is a function of the interaction between our genes, lifestyle choices and environmental factors. No single patient is alike—yet all of us will have some likenesses that we share with others.
Precision medicine is an approach to health management that takes into account where you live, what you do and your family history and genetic makeup (including any genetic mutation), giving health care providers the information they need to make customized recommendations for people of different backgrounds, ages and geographic regions.
With its emphasis on individual patients, precision medicine might seem to be a narrowing of focus. In truth, the knowledge gained from targeted therapy to the unique molecular or genetic mapping of individual patients inevitably leads to a more nuanced understanding of the patterns, progressions and occurrence of disease within populations.
That's why The Precision Medicine Initiative was launched in 2015. The partnership between the National Institutes of Health (NIH) and several other research centers was designed to "understand how a person's genetics, environment and lifestyle can help determine the best approach to prevent or treat disease."
In the short term, the goal of this Precision Medicine Initiative is to expand the precision medicine approach in cancer treatment. But the long-term objective of this precision medicine program is to make precision therapies a part of all disease treatment in the future.
Francis Collins, who led the Human Genome Project and is the director of the NIH, said that it's "a false dichotomy that you have to have either precision medicine or population health. It is not a conflict."
In fact, the one feeds the other. "Precision public health is about using the best available data to target more effectively and efficiently interventions of all kinds to those most in need," The Lancet's Editor-in-Chief, Richard Horton, posted in the esteemed journal two years before the COVID-19 pandemic.
In the event of future health crises, including the current pandemic, vaccine availability may literally drive life or death decisions. The insights derived from precision medicine will be invaluable for identifying which individuals within populations are most vulnerable, helping to determine who gets vaccinated first and thereby slowing the exponential spread and impact of virus.
Extracting and purposing the value within healthcare data from the individual patient to the population is being made easier by the tools and technologies of digital health.
Making Hay with DNA
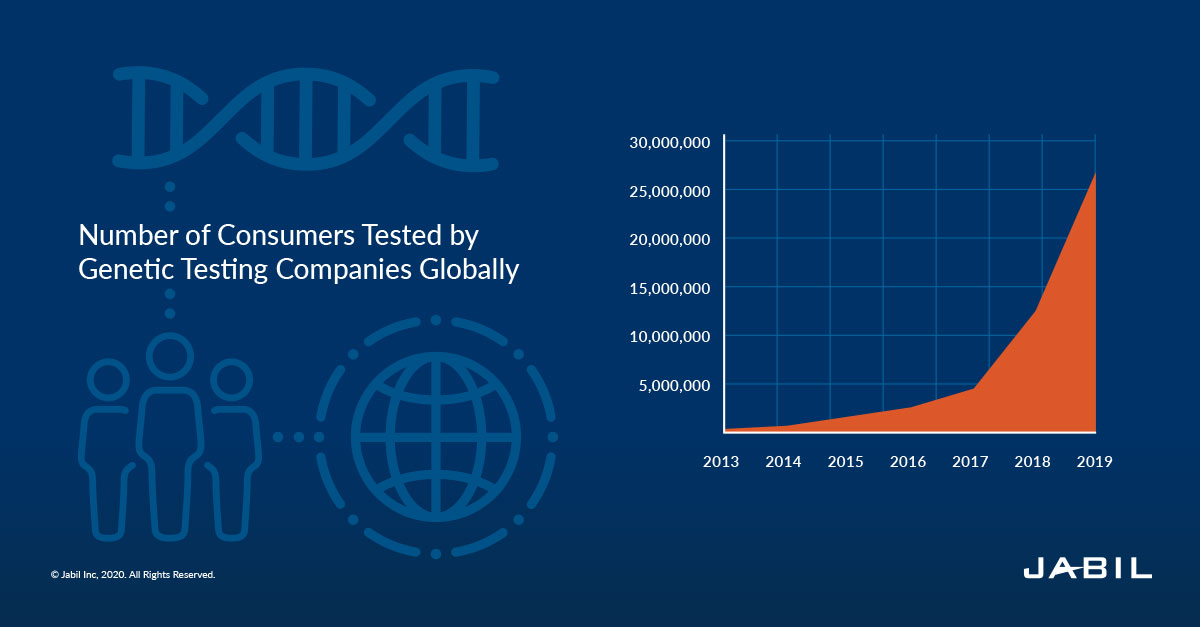
Every year more personal DNA data is being collected and analyzed for clinical insight than ever before. A company like 23andMe entered the market as a direct-to-consumer (DTC) provider of genealogy services but has been branching out recently with more focus on population health seeking to gain ground in the medical sector.
The DTC genomic testing leader has more than 12 million customers and collected over three billion phenotypic data points. In September 2019, 23andMe announced they had achieved the ISO/IEC 27001 standard for their information security management system. And in August 2020, it became the only company with direct-to-consumer pharmacogenetic reports cleared by the FDA.
Pharmacogenetics is the process of understanding what, if any, role genetics plays in a patient's reaction to drugs. The company's Personal Genome Service test analyzes DNA from a self-collected saliva sample, and the report describes if a person has variants in certain genes that may be associated with a patient's ability to metabolize some medicines.
Yet, despite milestone achievements like these, the rapid expansion in our knowledge regarding the 20,000–25,000 genes in the human body, the functions of the vast majority of genes and their variants are still not well understood. Companies vying for traction in this exciting and emergent space have a broad field of operations. In fact, the predictive genomics market has been predicted by some analysts to be a $2.5 billion market by 2025.
At one end of the spectrum is whole genomic sequencing, which looks at all 6.4 billion letters of the human genome, while companies like 23andMe focus on genotyping, which looks at less than half of 1% of that number. To the extent more is better in the world of Big Data, there is no more comprehensive genetic test than your whole genome. Accuracy and confidence in the process are vital when you consider, for example, that the analysis has the power to inform you of a predisposition to breast cancer or Alzheimer's disease.
When the first whole genome was sequenced in 2003, the process required 15 years of work, 20 different labs and more than $3 billion. Now companies like genomics start-up Veritas Genetics are working from a price point below $1,000 and the consensus is that sub-$500 or even $100 is not far off.
The downward cost trajectory of human genome sequencing at first aligned intriguingly with Moore's law. The pace of advances in sequencing seemed in sync with those in microelectronics. But tracing back over the last couple of decades reveals how the dramatic drop-off in sequencing costs has resulted in an equally dramatic acceleration of demand for genetic testing by consumers.
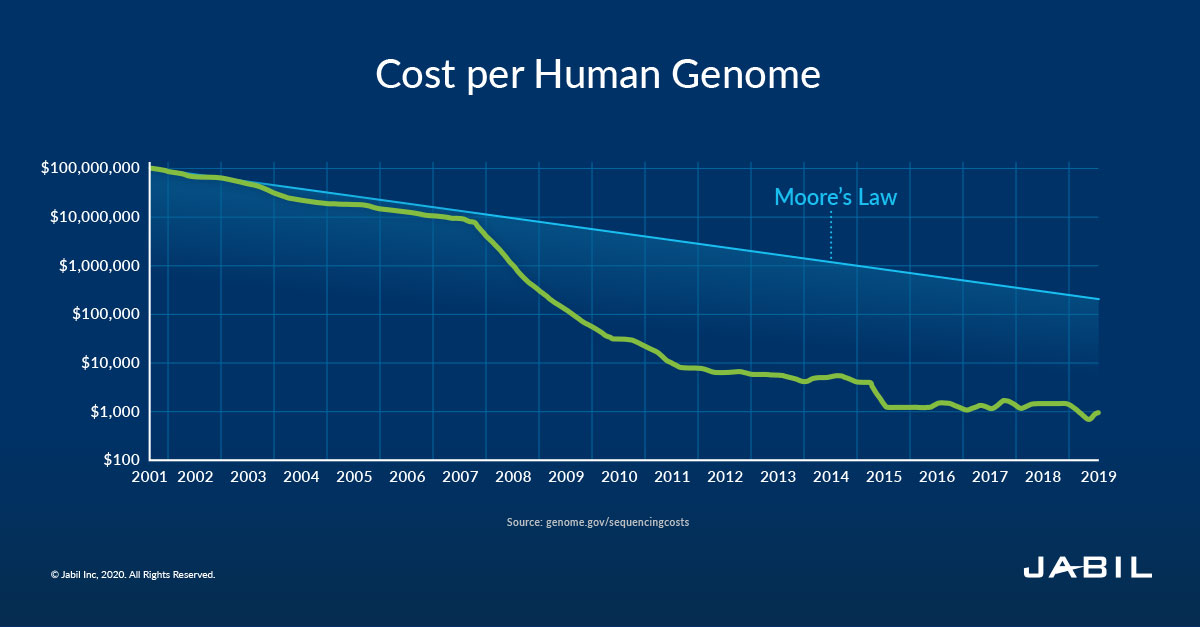
"This is the inflection point," Rodrigo Martinez, chief marketing officer for Veritas Genetics, said. "This is the point where the curve turns upward. You reach a critical mass when you are able to provide a product that gives value at a specific price point. This is the beginning of that. That's why it's seismic."
Predictive Diagnostics: Powerful Insights, Incredible Value
As sequencing technologies have helped decipher the human genome, other emerging technologies in diagnostics are helping to deliver even more valuable medical insight in support of predictive outcomes.
Imaging and microscopy technologies, for example, have revolutionized our ability to visualize and monitor cellular and molecular processes in cells and tissues. Mass spectrometry and array-based and microfluidics methodologies are helping to drive the rapidly growing knowledge base of molecular composition and the function of biological systems. Sophistication and precision are transforming diagnostics.
The increasing innovation in this space is impressive considering the headwinds diagnostics face within the United States due to a reimbursement environment, which remains cost-based rather than value-based. Yet, precision medicine is impossible without diagnostics. They are the essential guidance system of clinical practice, illuminating the path forward in pursuit of matching the right patient with the right precision medicine treatments at the right time.
Robust diagnostics accomplish and inform an invaluable range of clinical "signposts" and serve a key role in the health value chain by influencing the quality of patient care, providing predictive insights and better clarifying downstream resource requirements. From consumer-friendly at-home pregnancy and glucose monitoring tests to more complex automated laboratory-based systems, these tests are often first-line health decision tools and are irreplaceable for ascertaining Rx response and identifying potential adverse events.
As applied within oncology, diagnostics that precisely identify that a patient has a specific genetic mutation help guide clinical care while also informing life decisions faced by the patient, ensuring the most effective and personally appropriate long-term strategies for disease treatment or management.
Microfluidics devices enabled by lab-on-a-chip technology and integrated with sophisticated analysis equipment and Cloud-based apps facilitate the integration of measurement results into a personalized care regimen. This is just one example in which data and the tools of clinical decision support are synergistically advancing upon yesterday's technology for a more personalized and comprehensive level of care.
Point-of-Need (PON) testing is any diagnostic test performed away from reference laboratories - in other words, at home, at the patient's bed, in ICUs (Intensive Care Units), at the physician's office or near a production line. AI-enhanced blood testing devices that count blood cells are being utilized PON so that results can be received more quickly, with no sample transportation requirements, lab or phlebotomy services.
Doing a full blood count (FBC) using AI at PON is a big deal, reducing complexity, time, error and costs. The diagnostic device allows a healthcare professional to carry out an accurate test within 10 minutes from a finger prick and requires only minimal training.
Innovative diagnostics devices like these are remarkable for the utility they provide clinicians and providers as well as their exceptional ease of use at the patient level. Creating even more value moving forward will require a reconsideration of financial incentives as studies show that while diagnostics historically drive 70% of healthcare decisions, they have accounted for only 2% of total healthcare spending in the United States.
Follow the Jabil Blog
Sign up for weekly updates on the latest trends, research and insight in tech, IoT and the supply chain.
The Right Nudge at the Right Time
Christofer Toumazou is a professor of engineering and chief scientist for the Institute of Biomedical Engineering at Imperial College London. He's also the founder of an innovative company with an apt, simple and appropriately easy to remember name—DNA Nudge.
Starting with the assumption that DNA is not a choice, it's fixed, but other determinants of health are subject to our decision-making, initial research focused on medical conditions that can be impacted significantly by diet, like type 2 diabetes or heart disease. If you have pre-diabetes, then you need to be careful about foods that could cause a rapid spike in blood sugar. Likewise, if you have the hypertension gene, there's another quantifiable list of food you need to be careful about.
The process takes 15 minutes with a simple saliva swap and a small analytic diagnostic device and cartridge. It can be done in retail environments, like supermarkets, department stores or in their own stores, such as the flagship outlet in London. AI analysis integrates with a secure mobile phone app for scanning barcodes. The nudges - for products that are genetically optimal for you - are delivered at the touch of a button, and in the palm of your hand, making it easy for you to optimize your grocery cart for your own personal health profile and nutritional needs.
Companies like DNA Nudge are constructing a fascinating bridge across the psycho-social to our physiological selves, delivering a sophisticated technology, once limited to genetics laboratories, directly to consumers in hopes of improving lifestyle choices and guiding a better path towards wellness. Proactive, precise and predictive, DTC product solution innovations like these have the potential to accomplish an extraordinarily big lift with a simple little nudge. Genetic testing, predictive diagnostics and the other technologies driving precision medicine are in the final analysis just information, and not actualized prevention. The patient, in concert with clinical support and physician oversight must, as has always been the case, navigate their own way confronting what ails them in pursuit of improved outcomes.
Yet, we all have an untapped capacity for health. Digital healthcare products and platforms are making it easier than ever to tap precision medicine by encouraging healthier lifestyle choices, while also providing access to recommended medical interventions and assembling a fuller understanding of not only our own health but the well-being of us all. Personalized medicine is right around the corner.
Download the 2021 Digital Health Tech Trends Survey Report
Insights from over 200 digital health decision-makers on the barriers, opportunities and the future of digital health.


