Digital Healthcare Data: Where We've Been and Where We're Going

Some have called the innovation in healthcare a "Gutenberg moment." The first printing press sparked a technological revolution that eventually led to the computer you're reading this on. In the same way, new healthcare technology is reinventing several aspects of healthcare; individual medical products are becoming more portable, advancements in disease-state therapy are growing, and even the cost of sequencing a human genome has dropped by a factor of a million.
Remote patient monitoring (RPM) through wearable devices, healthcare platforms harnessing artificial intelligence (AI), fitness and wellness apps as well as telehealth (and its increased utilization throughout the pandemic), are all examples of the progress of the digital transformation in healthcare. These innovations are improving patient outcomes, making processes more efficient and cost-effective, reducing errors, and optimizing existing therapy delivery, all while helping lower healthcare costs.
Woven into every one of the trends and dynamics of the industry's transformation is healthcare data. Between existing medical records, legacy data not yet processed and new data being fed into the system every single day, there's a tsunami of health data being collected.
Current estimates suggest a single patient generates close to 80 megabytes each year in just imaging data within their electronic medical record (EMR). This data is multiplied by each new Internet of Medical Things (IoMT) technology, medical device, health tracker and even smartphone that are increasingly becoming a part of our healthcare infrastructure.
Additional factors driving data growth are falling digital storage costs, consumer acceptance of cloud-based services and subscription models, the ramp in adoption of electronic health (eHealth) and mobile health (mHealth), and wearable technologies, as well as recent government initiatives and regulatory mandates purposed to open up and democratize data sharing.
Data management and analytics are now mandatory competencies across the healthcare industry, catalyzing a whole series of mission-critical questions. Some of the most pressing questions include how to use data to improve health for individuals and the greater population, as well as how to protect data. Healthcare providers, pharma companies, established medical device and equipment OEMs, and non-traditional entrants to the industry are all taking vigorous steps to work through the answers to these questions to better position themselves for the future of global healthcare.
The Three Vs of Healthcare Data
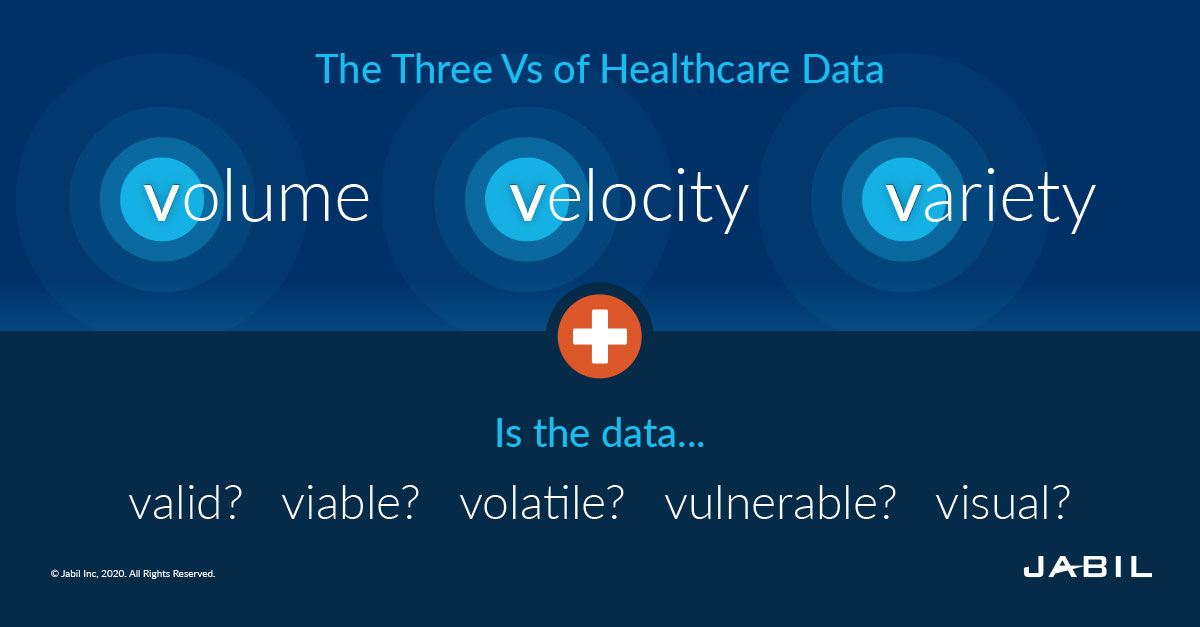
According to research and advisory firm Gartner, three words beginning with the letter "V" provide a helpful frame for understanding the term "big data": volume, velocity and variety. Gartner analyst Doug Laney came up with these three Vs back in 2001.
The sheer volume of healthcare data is growing exponentially and at an explosive rate. Velocity is proving itself as a differentiator in numerous industries. What about variety? Well, it's complicated.
There are two types of healthcare data. Structured data involves quantifiable values, using a national vocabulary standard or proprietary coding, such as EMRs; on the other hand, unstructured data refers to data that requires manual analysis and interpretation, such as physician notes and x-ray images.
In truth, the complexity of the modern healthcare system is at such a scale that it's necessary to enlist a few more letter "V" words to fully capture the challenge of extracting actionable insights.
Is the data valid; can we trust it? Is it relevant — or in other words, viable? Does it change often — volatile? Then there's vulnerability. What can be done to keep the data secure? And increasingly, particularly as a function of the volume of the enormous wash of digital files, how can key insights and analytics pulled from the data be rendered visually so that it's digestible for patient and provider alike in support of improving health outcomes?
Interoperability: Turning Healthcare Data Investment into Value
The objective of data interoperability within the healthcare setting is to build an improved system that will allow users to find, understand and act on information when they need it, regardless of the dataset. The status quo has been built upon proprietary structures and is hampered by their consequent incompatibilities.
Data is an extremely valuable commodity, capable of providing its "owner" with a competitive advantage. But building a healthcare system that will evolve at the rapid pace of technology and medical science requires a spirit of collectivism in which data becomes democratized. Without this, the challenge of delivering upon true interoperability will not be solved.
According to Jabil's Digital Health Technology Trends Survey, more than nine in 10 healthcare solution providers agreed that digital healthcare should be standardized to enable interoperability between devices and within product platforms from various brands.
Follow the Jabil Blog
Sign up for weekly updates on the latest trends, research and insight in tech, IoT and the supply chain.
Interoperability has been one of the hottest topics in healthcare for years. The situation has been considerably more complicated in the U.S. than countries like the U.K. or Canada due to the way the American health system has been balkanized by various vendors and proprietary formats.
In fact, there are two primary big names in the space today — Epic and Cerner. By some estimates, these companies control almost 50% of the total EMR market. Although competition between these vendors has been dynamic, even they have embraced data interoperability.
As elusive as it's been, true healthcare data interoperability is getting closer, and not a moment too soon. Many factors are driving change; consumers are demanding access to their own health information while technological advancements in web and mobile applications are opening up exciting opportunities. Most significantly, however, is the degree that recent governmental actions are helping to tip the scales.
In April 2021, long awaited rules from the U.S. Department of Health and Human Services (HHS)' Office of the National Coordinator for Health IT (ONC) implemented long-awaited final regulations aimed at enabling more widespread sharing of health information by healthcare providers and health plans to improve treatment, care coordination, public health and more. Both sets of rules emphasize patient access to their own health information and call on the healthcare industry to adopt standardized application programming interfaces (APIs) to facilitate individuals' access to their structured electronic health information using smartphone applications.
Under these new regulations, which data can be shared will be dictated more by individual patients' wants and needs and less by the standards set by HIPAA. In July 2021, HHS updated their interoperability standards to start collecting and considering data around social determinants of health in the clinical setting. This was intended to better serve the LGBTQ+ and other underserved communities — helping to create a higher quality and more equitable healthcare system.
This creates a tremendous opportunity and will be another catalyst for more innovation and competition in the industry by fostering an ecosystem of new applications to provide patients with more choices in their healthcare.
What's FHIR Got to Do With IT?
"FHIR" (pronounced fire) stands for "fast healthcare interoperability resources," which are informatics standards that enable data to move seamlessly from different sources to healthcare environments like electronic health records systems, apps and digital platforms. Debuting in 2011, the intent has been for HL7 FHIR® to cover essentially every healthcare data type that can be shared among industry stakeholders, simplifying communication and automating data processing across complex systems.
A decade later, version 4.0 represents a significant advance in accessing and delivering data while offering enormous flexibility and ease of development with a framework that leverages the latest web standards. This latest version also includes a RESTful API, an approach based on modern internet conventions and widely used in other industries. For patients and providers, its versatility can be applied to mobile devices, web-based applications, cloud communications and EHR data-sharing using modular components. FHIR is already widely used in hundreds of applications across the globe for the benefit of care providers, patients and payers.
"HL7 FHIR R4 is a beginning," said HL7 CEO Dr. Charles Jaffe. "It is the legacy of eight years of innovation and collaboration among a community of thousands around the world. It is a commitment from HL7 to create a platform from which interoperability can someday emerge. It is a promise to provide reusable data across the continuum of biomedical research, patient care and population health.
One high profile and early leverage of HL7's FHIR standard is Apple's HealthKit app, available on the iPhone and Apple Watch. Launched in 2014, this was the company's first major foray in the health technology market. The HealthKit app integrates information from multiple sources, including data collected directly by the Apple device as well as clinical health records like EHRs.
Apple's implicit support for improving data sharing among patients' various healthcare touchpoints provided FHIR momentum. Seven years later, there's substantial evidence that data has become increasingly liquid — capable of flowing across the health system.
Industry and regulatory bodies, as well as healthcare businesses, have now united around the FHIR standard for data exchange and the U.S. Core Data for Interoperability (USCDI) as the standard for capturing data. It should be noted that there are different implementations of FHIR APIs, as well as other minor ambiguities for developers, but the larger story is that at last, the long-standing technical barriers to interoperability are finally being breached.
It's a topical and timely story, too. Response to global pandemics like COVID-19 cannot be fully optimized without comprehensive data that can be seamlessly shared across a broad partner ecosystem. Perhaps the most exciting feature of data interoperability at this level is that ideas from all over the world can be built and tested with the FHIR standard, delivering on the loftiest of goals for population-wide health strategies and eradicating the devastating toll of chronic disease in all areas of the globe.
Who's on FHIR?
Open APIs in healthcare have led to contributions across the entire industry landscape, including non-traditional healthcare players whose enthusiasm and skill in developing innovative applications for all imaginable healthcare niches is already on display in the marketplace. Many of these companies also bring well-honed customer engagement credentials to the healthcare arena.
Big names like Microsoft, Google, Amazon, IBM, Oracle and Salesforce are building FHIR servers and integrating with FHIR data, but small teams also have the opportunity to get on board and begin to constructively provide and consume data for a large variety of applications.
Bringing a digital healthcare platform to market requires more than the expertise of a single solution provider. Cross-industry collaborations are a must-have in order to deliver the requisite scale needed by AI and machine learning to effectively power precision medicine and drive advancements in population and disease-state care. The more alignment, the more data, the better the overall system — for everyone. Limitations just mute the tremendous benefits that are now within reach. The industry has all the tools at its disposal and the work of synching them all together has just begun.
In Seattle, the Fred Hutchinson Cancer Research Center is managing medical data from multiple hospitals and electronic health records systems for several projects engaging cancer patients with remote monitoring. The underlying platform architecture is Microsoft's Azure API for FHIR. By facilitating the integration of all the various fragmented data streams into a useable format, the FHIR architecture gets the Center's cancer researchers to the next step: unlocking the power of AI to determine actionable healthcare analytics and insights.
Privacy Concerns Are a Formidable Obstacle
Of all the potential obstacles to this great leap forward, however, protecting patient data and privacy remains front and center. It's one of the most pressing concerns for healthcare decision-makers in the Jabil survey. In fact, close to half of the participants identify privacy concerns as a major factor hampering the adoption of their company's healthcare solutions, with companies in North America and Europe most frequently reporting these worries. The same percentage, 43%, say they are building new teams with technology and data expertise to manage these issues.
Moving forward, healthcare IT needs to figure out how to have it both ways: seamless data exchange while maintaining and building public trust in the industry's ability to keep private information safe and secure.
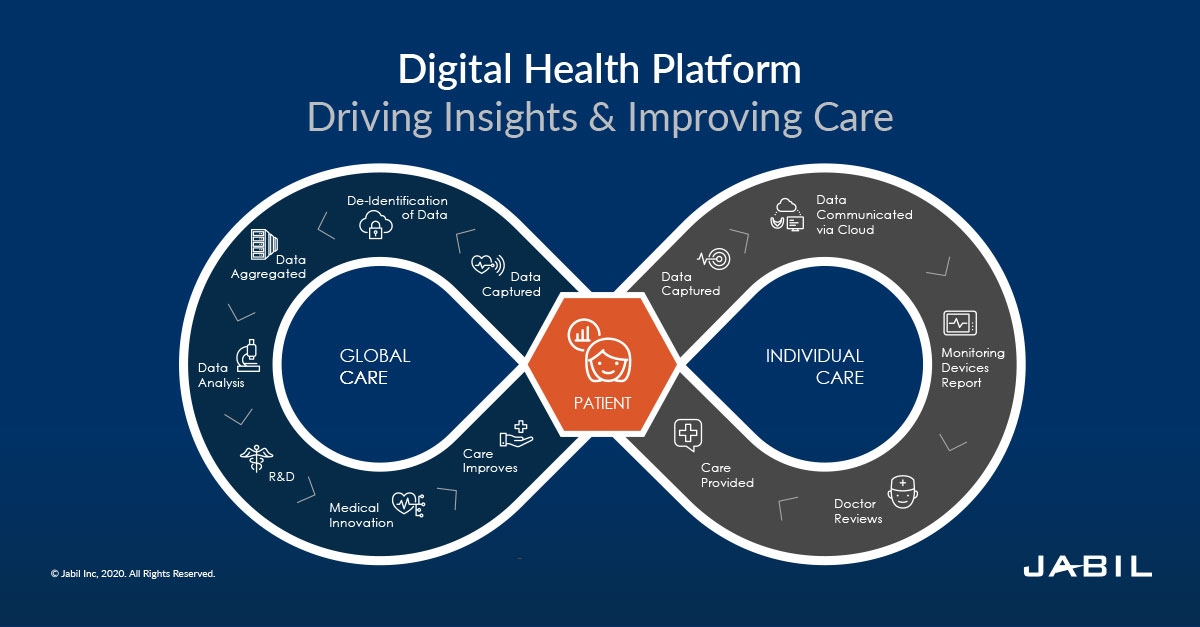
The Payoff Is the Platform
At the heart of all of these industry efforts with data is the drive to enhance knowledge and access. It's about illuminating the darkest parts of our pursuit of health and wellness and securing the most informed patient care from our providers. Digital health platforms will increasingly supply the staging for this pursuit. They also provide the means for evolving models of engagement with new opportunities to diversify revenue and otherwise broker between upstream and downstream stakeholder segments eager to transact upon the value inherent in digital health data.
According to the Jabil survey, 17% of participants are already pursuing data-based revenue streams. Another 43% are seriously considering their options.
In many ways, patient health records have been reluctant to leave the 20th century while the rest of us have moved well on into the 21st. We are now a highly mobile and connected society that's become accustomed to seeing whatever information we want — including our workout data, steps taken and calories ingested — displayed on whatever device we choose. Quite often that device fits in our pocket or on our wrist and stays tethered to us 24 hours each day — literally, in the case of wearables.
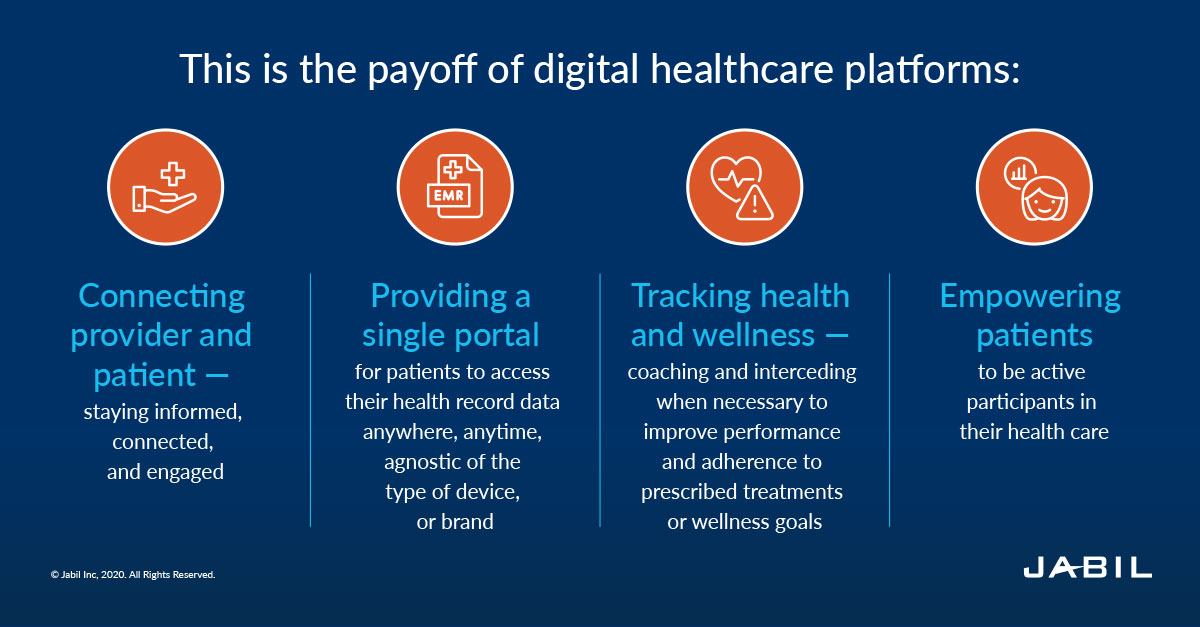
We'd also like all this information to be presented engagingly, accessible and shareable. This is the payoff of digital healthcare platforms:
- Connecting provider and patient — keeping them informed, connected and engaged
- Providing a single portal for patients to access their health record data anywhere, anytime, agnostic of the type of device or brand
- Tracking health and wellness — coaching and interceding when necessary to improve performance and adherence to prescribed treatments or wellness goals
- Empowering patients to be active participants in their health care
Data management has also become sophisticated enough that current models can deliver key insights into the impact of non-clinical factors, like food insecurity and unemployment, on patient outcomes. These psycho-social factors, often referred to as social determinants of health (SDH), are providing a much richer view on how to prioritize finite resources and better ensure no one is disadvantaged in their pursuit of health due to economic status or other socially determined circumstances.
Healthcare OEMs are at a crossroads: Either make significant investments in their own data processes or look to collaborate with partners for that build-out. It's not enough to be in possession of data; it must be collectivized and managed so that its power for actionable insight is made whole. Big data offers healthcare a limitless future, and increasingly, it's nudging us forward to a more proactive and predictive management of health that will genuinely deliver improved quality of life for us all.
Download the 2021 Digital Health Tech Trends Survey Report
Insights from over 200 digital health decision-makers on the barriers, opportunities and the future of digital health.